
An Understandably Dramatic Story of How Necrotizing Fasciitis Nearly Killed My 23-Year-Old Daughter.
“Mom? My ass hurts.” The phone call that started it all. A few questions and answers later I’d diagnosed my kid quickly with her second time Pilonidal Cyst. I told her to monitor it and to call for a doctor’s appointment. As is common for Kendra, I got pushback.
Her first Pilonidal Cyst had happened when she was living halfway across the country in Wyoming where she’d done well establishing medical care. Once she moved back home to New Hampshire a little less than a year ago she left the insurance and routine medical care behind. “I don’t have insurance. I don’t even have a doctor.”
Kendra is complex, disabled and not often organized – she had prioritized a new relationship and bouncing around the state with the former boyfriend over caring for herself and reestablishing her medical care. She was diagnosed with her first developmental disability at the age of 3, and several more mental health and intellectual disabilities over the following 20 years. She is also a Type 2 Diabetic, and her Diabetes had gone unmanaged for the last year. All of this would come back to haunt her, but more about that later.
Eventually, the pain became intolerable and she went to the emergency room on Sunday, August 4th. Here, the story divides. In her version, the emergency room doctor refused to lance the cyst, gave her an antibiotic injection and a prescription and sent her on her way with no instructions on how to properly care for th cyst. In another version, as documented later in her medical charts by a different doctor, she had refused to have the cyst lanced during that first visit to the ER. I intend to get to the bottom of this part of the story in the very near future, but for now, there is too much on my plate.
I picked up her antibiotic prescription and dropped it off to her. When I walked in, and I’ll never forget this for as long as I live (because hindsight is 20/20), her then boyfriend said, “Sorry if you heard me being a dick, I’m just trying to get her to understand she’s not helping herself by crying and screaming and that it’s just stressing her out worse.” I mean, I guess that seems reasonable – and I didn’t hear him being anything from outside the door so I lacked context. Kendra’s nickname is “Kendrama” and for good reason – she is, and always has been, dramatic. And, I do mean over the top, with exceptional flair and added affect. But, I digress.
I handed her the meds, gave my best rounds of mom advice (hot compresses, take with food, hydrate, alternate Tylenol and Motrin, keep in touch). Hugged and kissed her, told her to get better and left her in the care of … a monster. But, I’ll get back to that, too.
The vomiting began shortly after she got home from the emergency room. We assumed it was a response to the antibiotic injection. As she continued to take the antibiotics, she was unable to keep anything down and her pain continued to increase. On Tuesday, August 6th, the Pilonidal Cyst burst. I was even lucky enough to received photographic evidence at 7pm that evening. Something I would later be so glad to have.
When Kendra called to tell me I said, “This is the beginning of the end, now you can finally get some relief.” I. Ate. My. Words. I ate them so hard, I’m still digesting them over three weeks later and the indigestion is unbearable. This was the beginning of a nightmare.
After the cyst opened I gave my mom advice again, keep it clean and dry. Keep taking the antibiotics, the pain relievers and keep hydrating. But, the vomiting continued and the pain increased. The cyst continued to ooze, and the inflammation began to grow. I received another photo on Wednesday morning at around 10 am and could see that there was some irritation and redness, but I’m not a doctor. I suggested we keep a close eye and consider going to the emergency room if it gets worse. Two hours later, another photo. I immediately called Kendra and told her she needed to go straight to the emergency room. Something was very wrong. The center of the cyst had turned black and the redness was expanding and the swelling increasing. This was not the relief we anticipated. My husband wasn’t home at the time so I couldn’t pick her up and take her so we brainstormed a ride for her.
She called soon after, in tears. “Mom, I need you. They might have to do surgery. I’m going for a CT scan.” I said I was on my way, hung up the phone and my husband and I went to the hospital. By the time I arrived, the CT scan was done and the surgeon was in the room explaining the surgery and the risks. I still did not know or understand the magnitude of what we were dealing with at that point. In fact, neither did the surgeon. He said that there was a risk of death, but I assumed that was just something that they said to everyone before an emergency surgery to cover their asses in the event something went wrong.
My baby is 23 years old, she had a little cyst, she’s not going to die for heaven’s sake.
The surgeon explained there was gas around the wound on the CT scan. I didn’t know what that meant. He anticipated the surgery would take 45 minutes. He expected she would be in a great deal of pain and that she would be intubated for a day or two to help manage the pain. That seemed a bit excessive, but what did I know? Nothing. I literally knew nothing. Kendra was in tears, she called my Mom, my husband left to pick up her Dad and bring him back to the hospital so we could all be by her side, and then she said, “I think I need a priest.” There was an urgency to get her into the surgery, and not enough time to get a priest into the hospital so I FaceTimed our nephew, who happens to be a Pastor. I couldn’t explain to him the gravity of the situation – in part because I didn’t understand it, and in part because I didn’t want to solidify it. But, he talked with her and he comforted her.
They rolled her off and I, her Dad, Step Dad and the former boyfriend, made our way up to the surgical waiting room. A short time later someone came out looking for me, Kendra was all prepped but was asking for her Mom. I went in to give her love, hugs, and reassurance, to see her in that hospital bed so scared and trying to be brave, listened to the anesthesiologist explain that she’d be getting a central line because “she’s pretty sick” and then hugged my baby girl, told her how much I loved her, and heard her tell me she loved me “soooo much mummy.” I had no idea in that moment how desperately I would cling to those words, and how much I would beg to hear them again.
Three hours later, the surgeon found me pacing the hallway outside the surgical waiting room. “Erica, is the family in here?” Fuck. He sat down in the waiting room and he was upset. The infection was more invasive than what he saw on the CT scan. He kept cutting and cutting and cutting and couldn’t get to healthy tissue. There is necrotic tissue from her tailbone to her vulva. There is gangrene. She may need a colostomy. She needs a full trauma team. A better facility. I can’t keep going without hurting her. Her blood pressure dipped during surgery. Fuck. Fuck.
Fuck.
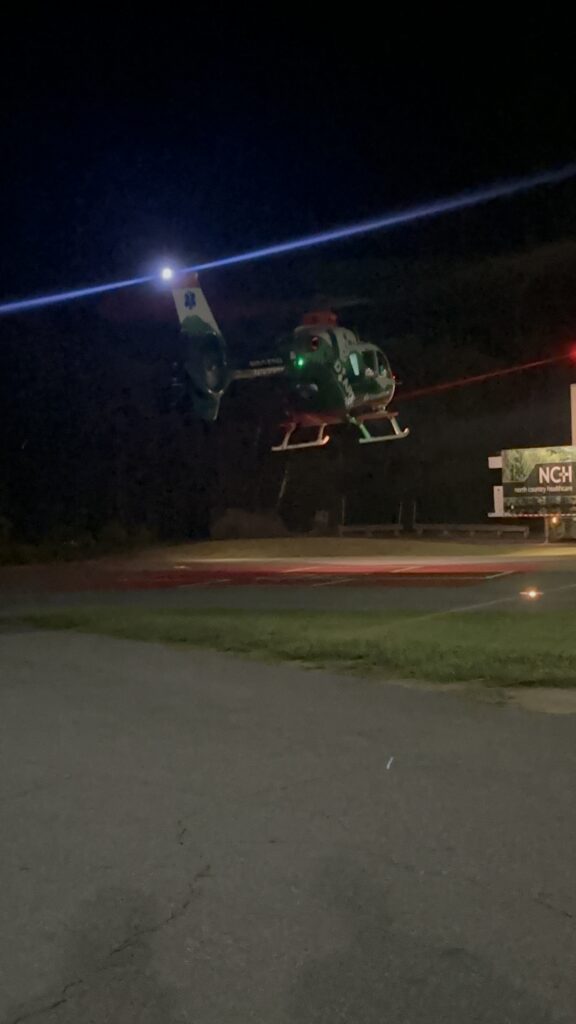
He put in some calls and found a Level 1 Trauma Hospital that was best suited to care for her that had an open bed and was willing to accept her case. He almost begged them to take her, and had emphasized to them that she was just 23 years old. Just twenty-three years old. She was going to be moved from the OR to the ICU while waiting for transport. There were no helicopters available. They were going to have to send in a fixed-wing aircraft. They can’t wait, she needs to be moved. They found a helicopter.
We called in some family to see her before she left. My parents, her father’s mother and sister, her bestie/cousin who’s just 10 days younger than her. We FaceTimed her brother and Sister in Law out of state. I ran home to pack a bag naively thinking they’d let me on the helicopter with her. They definitely did not.
I held her hand, I kissed her forhead, I watched her monitor, I sang to her, I waited, and I hardly breathed. I cried, and I begged the universe to save my girl, I made ridiculous promises that I’ll have to keep if I could just keep my kid. I asked the doctor if she was going to be okay and his words are acid etched into my soul,
“I can’t promise she’s going to be okay but I can promise she’s going to be in the best hands.”
There are no words to describe the feeling you get when watching medical professionals put your baby on a stretcher, into a helicopter and then seeing that helicopter lift off and eventually disappear at 1 am into the dark night not knowing if you’ll ever get the chance to hear your little girl’s voice again. I’ve spent almost 3 weeks at this trauma hospital where these helicopters land over and over all day long bringing people in from all over New England – the worst-case scenario patients who need the best care, the … best hands. Every single time I hear those helicopters my heart rate speeds up, my breath gets caught, and my eyes turn to faucets. I try to tell myself that the helicopter was a hero in our story, that it was the Batmobile flying her off to safety – but these are just words I say.
The helicopter now is symbolic of that moment of fear, helplessness, desperation, and brokenness that feels unlike anything I have ever known before. The helicopter is a trigger for the PTSD I know I walk away from this experience with. The helicopter is a reminder of how my baby girl was nearly whisked away from me forever.
The hospital is about 3.5 hours or just under 200 miles from home. I was told that I wasn’t allowed to go into the ICU to see Kendra until 11 am, something I learned was part of an extremely strict visitor policy at the hospital and one that is really challenging to get around. Because, I definitely tried. My husband and I made the drive down not knowing what to expect, where we would sleep, what would happen next. I was leaving everything up to chance, and if I had to become unhoused in the city to be by my daughter’s side through this, then so be it.
Seeing Kendra in the ICU for the first time that morning, on August 8th, was complex in terms of emotions – relief that she was still alive, disbelief that she was in this situation. I began talking to doctors, nurses, specialists, surgeons, social workers, etc. etc. etc. And the medical terms started flying.
Necrotizing Fasciitis. Gangrene. Sepsis. Life Support. Vasopressors. Serial debridement. Diverting Sigmoid Colostomy. Deep vein thrombosis. Urinary retention. Wound vac. UTI.
The Pilonidal Cyst became infected with Group A Streptoccocus (think Strep Throat) and turned into Necrotizing Fasciitis. Necrotizing Fasciitis, also known as “flesh eating bacteria” is a” serious life-threatening infection with mortality rates ranging from 20 to 80%.” Her untreated diabetes worked like fuel on a fire with the blood sugars feeding the bacteria creating a perfect storm of advanced destruction. The mortality rates for Necrotizing Fasciitis increase with comorbidities such as diabetes by drastic measures.
The first surgeon knew that the first line of defense is to remove the necrotic tissue and stop the spread of infection surgically as quickly as possible. His urgency to get her into surgery was not without significant grounds. Unfortunately, he soon found that there was more damage, and more work to be done. Cue the ‘copter.
Kendra was on life support from Aug 7, 2024 until August 12, 2024. During this time, I heard things like, “she’s very sick” and “we’re just taking things hour by hour with her.” I can recount every single second and yet, all of it is a streak and a blur. A period of time forever embalmed and solidly cemented in my consciousness … looming in the dark spaces of my core memory bank daring me to take a single thing for granted again.
She was monitored, poked, prodded, and taken into the operating room for serial debridement and irrigation. Eventually, the wound was cleaned enough to allow for vacuum-assisted closure (VAC), aka negative pressure wound therapy, a wound dressing technique that uses suction to help wounds heal. This has been exceptionally helpful, although it has not been the most pleasant for Kendra to deal with.
As I write this, we’re on day 19 and she’s having the debridement, irrigation and dressing changes that we call “vac changes” every three to four days with a plan to move them to weekly. She’s been in the OR and/or had one of these painful procedures more than eight times and counting. Most recently, a plastic surgeon consulted and will attend her next vac change to assess the wound and make recommendations for the next steps which might include a sacral flap surgery. This surgery would require additional hospital time and a very specific “turning” regimen – none of which sounds desirable, but, it would also shorten the overall healing time. Kind of stuck between a rock and a hard place on this. He’ll evaluate and she’ll follow up with him in a few weeks to make a decision. That means, for those few weeks at least, the vac changes will continue on as planned.
The day before Kendra came off the ventilator was one of the scariest as her lungs were degrading and starting to fill with fluids. Her vital signs were not doing great, either. It was clear that she was in a tough situation and her team needed to get her off the ventilator as quickly as possible. The respiratory therapist gave her a trial and she failed and they were unable to take her off the ventilator. She was in danger of hospital-acquired pneumonia and that would have been extremely difficult to overcome. My poor baby had so many tubes, ports, wires, alarms, monitors, and was so sick, she didn’t need a single ounce more trouble.
The next morning, Monday, 8/12, my husband got on a train to head back home. Our youngest kiddo just moved into his college dorm and my husband went back to spend his last week with him and make sure he was ready to go and then he and my Dad brought him to move in day on 8/21 and my husband joined me back in the big city. Anyway, that morning, I left my husband at the train station and walked to the hospital and into Kendra’s room knowing they’d planned to try to take her off the vent again that morning. When I walked in and saw her on the ventilator, my heart sank, the tears flowed and I felt like I was the only person left on the planet – 100% completely alone, broken and so incredibly weak.
But, by the grace of God, or good luck, or whatever it is that makes miracles happen when you least expect it, it was only a matter of timing and within the next few hours, my little girl opened her eyes, and the tube was taken out. She was awake. And in terrible, excruciating pain.
So much pain. Strangely enough, she complained first about her left leg hurting. Let me back up for a second and expain her wound. Remember this all started with a Pilonidal cyst – “A pilonidal cyst is a small, sac-like pocket that forms in the crease between the buttocks, close to the tailbone.” Okay, so basically, the top of the butt crack, right. And, here’s the medical terminology for what we started with:
CT pelvis obtained showing gas containing collection posterior to coccyx measuring approximately 8.3 X 6.6×6 X 4.6 cm.
By the time she was in the helicopter the primary wound was approximately 23X24cm or about 9” with three smaller incisions that were about 1×2 inches. Before the wound vac closed it all up? Over 12” – a square foot of open tissue in her sacral area. The infection spread from her tailbone to her labia. This created some complications that we are still learning about in addition to the infections and the wound itself. But here’s what we do know, and bit of what’s been going on:
- Kendra had to have a laparoscopic Diverting Sigmoid Colostomy. She now has an Ostomy bag. This may be able to be reversed someday, but for now, this is her new normal. We’ve been receiving education from the Ostomy nurses on staff at the hospital and it has been going well. Because of Kendra’s injuries and pain, I have been doing most of the learning, and I’m now able to change and empty the ostomy bags with some degree of confidence.
- Kendra has foot drop, or .. something. Remember she woke up complaining about leg pain? She also can’t feel her left foot or move her left toes. Physical Therapy and Neurology are working to get to the bottom of it (no pun intended), but we aren’t sure if she has permanent nerve damage caused by the flesh-eating bacteria, or if there’s something else going on, possibly from laying in bed so long. There is hope that even with this condition she will be able to walk with a special walking boot, and hope that it will resolve itself but, it’s being worked on.
- Kendra can’t pee. At least, not yet. They removed the Foley Catheter for one day. Although she still isn’t able to get out of bed, they have external catheters and eventually a bed pan that they can use but they wanted to get the catheter out for Kendra’s benefit. Unfortunately, the trial removal failed and the Foley had to be reinserted. There’s some concern that there could potentially be additional nerve damage connected to the wound contributing to the urinary retention. This is being monitored closely. And, to add to the bucket of good times, just yesterday they diagnosed a Urinary Tract Infection and started a new round of antibiotics.
- Kendra has Deep Vein Thrombosis. Her poor veins really have been through it. She’s had every single one of them poked and prodded and things going in and blood coming out … she had a central line put in at the first hospital, IV’s in both arms in the ICU (at the same time), an arterial line, constant blood sugar pokes … so much. Well, they took the central line out and within a few days her right hand swelled up a lot and started bruising from her elbow to her fingers. They did an ultrasound and confirmed that she had a blood clot in her jugular vein where the central line was. Sigh. This girl.
- Kendra has tired veins. This also meant that she could no longer have any blood draws, IVs, or blood pressures done on her right arm. And, the options for those things on her left arm were fading fast. Her veins are tired! A PICC line was placed in her left arm and a chest x-ray showed that it was slightly too deep so it was adjusted and seemed to be working well – until it occluded. Thankfully after two attempts, the IV team was able to dissolve the clot.
- Kendra’s Blood Pressure and Heart Rate Kind of Suck. After days of fighting to keep her pressure up, we’re now dealing with frequent blood pressure spikes. And, her blood pressure has to be taken on her leg because of the DVT in her right arm and PICC in her left arm. Her heart rate spikes when she is anxious and when she is in pain. She’s also been having increasing anxiety attacks. Thankfully, this hospital is super comprehensive in that they have a full team of specialists with the psych team staying on top of the anxiety and all of her nursing notes mentioning providing emotional support.
- Kendra’s lungs are still recovering. After 18 days, she is finally able to breathe room air, but it’s been a struggle to get her there. The bottom lobes of both lungs have been collapsed due to inactivity and from being on the ventilator for so long. She required supplemental oxygen through a nasal cannula 24 hours a day. Right now she’s doing well tolerating room air as long as she’s not moving (and she can barely sit up right now so, she’s not moving much), and her pain is fairly controlled.
- Kendra is an Insulin Dependent Diabetic and she gets it now. She has apologized over and over and over for “not taking care of myself.” I keep telling her this is not her fault, and it’s not, but that yesterday is over and done with but we can take the lessons we learned from it forward. She’s seeing how difficult her diabetes has been to manage and control with an entire team of specialists working on it. It’s not easy. But, she’s also seen the worst-case scenario both, here in what she’s going through, and for her Dad who is a failed kidney transplant survivor that has been on dialysis for over a decade due to complications from uncontrolled diabetes. Diabetes is not a joke, it’s not just about skipping dessert or taking your medicine so you can eat a cookie. If you or someone you know has diabetes, please, please, please take it seriously and get the education and support that you need to ensure that it is well managed. Blood sugars over 200 can create absolute chaos.
- Kendra is a Domestic Violence Survivor. (Trigger Warning) There are a lot of things you think about while your (adult) child is in an induced coma, including what you’ll talk about when they wake up. You probably won’t imagine that you’ll have to listen to her tell you about the abuse she suffered at the hands of yet another “man” that promised he would take good care of her, that he loved her, and that he wasn’t “like the others.” I mean, I already had my concerns about control and narcissism – like the real kind, not the generic label people tend to use … I’ve seen the thankfully now ex-boyfriend drive wedges between Kendra and her family and friends, and refused to allow that to become a thing for me. But when we started to talk about the boyfriend she said something that gave me pause and I gave her the room to open up a bit. When she did, the blood in my body boiled. The night before she was admitted to the hospital she had been crying in pain and the monster was apparently tired of hearing it. When he told her to “shut the fuck up” and she didn’t … he got on top of her and choked her out. And, this was not the first time. So, while her body was going septic and starting to shut down, and she was in absolute horrific pain … he choked her out. He. Choked. Her. Out. 24 hours later she almost died from the thing that made her cry … goodbye and good riddance to that evil, vile, disgusting, monster.
And so, we still have a long road ahead. Yesterday, Kendra sat up in bed for the first time. The pain that she has suffered has been almost unbearable at times and she has been immobile. Even if she didn’t have the pain she has the foot numbness to overcome, and almost three weeks in bed that will now require her to regain her strength. We’re not sure when she’ll be discharged from this hospital but we know the next stop isn’t going to be home – it will be a rehabilitation facility, first. Some obstacles to overcome, but she’s a fighter, she’s resilient and she’s so strong. And, I’ll be here with her every baby step of the way, hour by hour, and day by day.

She’ll be okay, because there’s no other option.
Our theme song for this fight: Rise Up by Andra Day. Kendra didn’t know that I had asked people to play this in her honor on an especially hard day while she was on life support. Shortly after she was awake, maybe a day or two after the tube was taken out, she asked me to play this song. Kismet? Maybe.
If You’d Like to Help
Please share this post and/or the fundraiser if you’re able, and donate if possible. We’ve been raising money through GoFundMe to help offset some of the costs associated with me being out of state, missing work, and being at Kendra’s bedside advocating for her and helping her to understand all that is happening while also providing her with love and support as she continues to get the medical attention and care she needs. Any additional funds will go toward helping her rebuild her life from needing to replace her bed and clothing to just generally getting reestablished in her own place once she’s strong enough to leave the home nest again.
You can also send donations directly through Venmo here or CashApp here.
Finally, one more way you can help is by shopping for Kendra on her Amazon wish list. These are items that will be needed for care as she moves into rehab and then once she is home, with a few fun things mixed in for her support and to cheer her up.


I love you both so, so much! I wish I could be there to hug you both!
We love you so much and can always feel your hugs wrapping us up tight no matter how far away you are! I’d be so lost without you, Mom!
Hi Erica,
I’ve been keeping up with Kendra’s progress through your FB posts. It’s amazing how fast things happen medically and it’s so refreshing to know that she’s progressing. I want to let you know that if I can help you and/or Kendra with anything please don’t hesitate to reach out. I would be so happy to help in any way I can!
Thank you, Reshea! I appreciate your kind words and your friendship. I will definitely reach out if needed! xoxo
Sending all the love. So glad Kendra is understanding how serious her healthcare is. Thankful she has you. 💚
So thankful WE have YOU! We are forever grateful for your love and support through this and all the things. Love you!
Erica, where are you? I’m here in Boston. Please contact me through Facebook. xoxo
Thank you, Jenny!! So much love and appreciation going your way!
Oh Erica! My heart breaks for you. It’s terrifying when you don’t know the details and don’t know if yours gonna get to keep your baby. I am sending great BIG hugs and Lots of LOVE from Indiana to you and Kendra.💓 She’s a fighter and she’s got her biggest fan and cheerleader cheering her on by her side. Keep up the fight Kendra ♥️
Awe, Robin – I watched and learned a lot about the Mama Bear fight from you! We’ve got some Super Sara energy going on over here. <3 Big love to you!! Thank you!!